4-5 Month Old Sleep: Consolidating Naps & Establishing Consistent Routines
Welcome to the fifth installment of our infant sleep series! The 4-5 month period often brings welcome stabilization after the challenging 4-month sleep regression. For many families, this stage marks the beginning of more predictable sleep patterns and the establishment of a more consistent daily rhythm.
Click here if you missed the 3-4 month old sleep guide.

4-5 Month Old Sleep Development
As your baby moves through their fifth month, several important sleep developments typically emerge:
- Post-regression stabilization: Many babies settle into more predictable patterns after the 4-month regression
- Nap consolidation: Transition from frequent short naps to 3 more defined, longer naps
- Extended night sleep: Potential for 6-10 hour consolidated night sleep stretches
- More consistent timing: Sleep and wake times become more predictable
- Consistent sleep cues: Clearer, more reliable tired signs
- Strengthened circadian rhythm: More defined day/night patterns with stronger biological sleep drive at specific times
Typical Expectations for 4-5 Month Old Sleep
During this age range, average sleep patterns include:
- Total sleep: 12-15 hours per 24-hour period
- Night sleep: Typically 10-12 hours with 1-2 feedings for most babies
- Naps: Usually transitioning to 3-4 naps totaling 3-4 hours of daytime sleep
- Awake windows: Approximately 1.5-2.5 hours between sleeps, with longer periods of wakefulness as the day progresses
- Bedtime: Often settles between 7-8pm for optimal sleep
- Morning wake time: More consistent, typically between 6-7:30am
Nap Consolidation: The 3-Nap Schedule
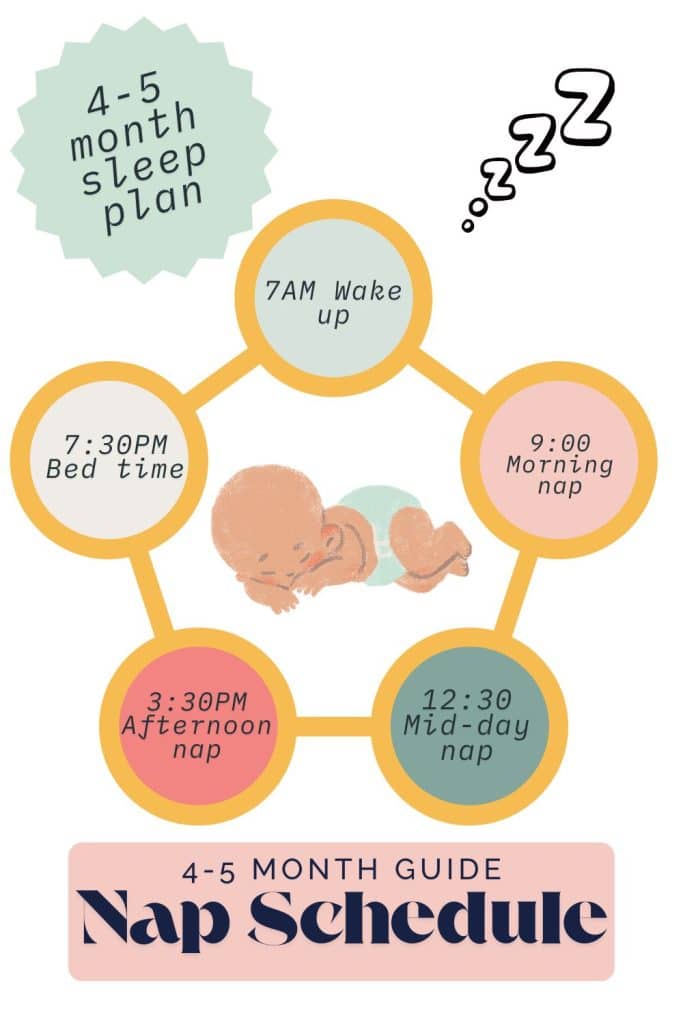
A significant development during months 4-5 is the transition toward a more predictable 3-nap schedule:
- Morning nap: Typically 1.5-2 hours after morning wake-up
- Midday nap: Often the most restorative, approximately 3 hours after morning wake-up
- Afternoon nap: Usually shorter “bridge” nap to reach appropriate bedtime
- Nap duration: Ranging from 30 minutes to 2 hours, with midday often longest
This rhythm generally emerges naturally but can be gently encouraged through consistent wake windows and environmental cues.
Building on Self-Soothing Skills
For babies who began developing self-soothing skills during the 4-month regression, this period offers opportunity for reinforcement:
- Consistent sleep onset: Continuing to place baby down drowsy but awake whenever possible
- Pause before responding: Extending brief pauses when baby stirs to allow self-settling
- Security objects: Safe loveys or comfort items may become increasingly important (always following safe sleep guidelines)
- More independent naps: Some babies begin taking longer, more independent naps in their sleep space
- Reducing sleep associations: Gradually minimizing associations that require parental intervention
For babies still working on these skills, this more stable period often proves easier for introducing gentle sleep training compared to during the regression.
The Importance of Consistent Routines

Consistency becomes increasingly important at this age:
- Bedtime routine: A predictable 20-30 minute sequence helps cue the brain for sleep
- Nap routines: Abbreviated versions of bedtime routine (5-10 minutes) help signal nap time
- Consistent sleep space: Using the same environment for all sleep periods reinforces sleep cues
- Regular timing: While not rigid clock-scheduling, aiming for similar timing each day
- Light exposure patterns: Bright light in morning, dimming as day progresses
- Energy regulation: More active play early in wake windows, calmer activities as sleep approaches
These consistent patterns help strengthen circadian rhythms and build sleep pressure at appropriate times.
Common 4-5 Month Old Sleep Challenges
Despite improved stability, several challenges often emerge during this period:
Nap Transitions
- Short naps: Some babies still take 30-45 minute naps as they master connecting sleep cycles
- Nap resistance: Increased awareness can lead to FOMO (fear of missing out) and nap resistance
- Late afternoon struggle: The third nap often becomes challenging to achieve due to being overtired by the end of the day
- Variable nap length: Day-to-day inconsistency in nap duration
Early Morning Wakings
- Sensitivity to light: Increased sensitivity to early morning light
- Hunger: Growing babies may wake from hunger earlier
- Overtiredness: Paradoxically, overtiredness can cause earlier waking
- Sleep pressure: Insufficient daytime sleep affecting morning wake time
Teething and Development
- Early teething: Some babies show first signs of teething discomfort
- Motor development: Practicing rolling, reaching, and other skills during sleep periods
- Increased awareness: More interest in environment can distract from sleep
Managing Early Morning Wakings

Early waking (before 6am) is common at this age. Try these strategies:
- Room darkening: Ensure blackout curtains block early morning light
- White noise: Consider continuing white noise through early morning hours
- Temperature check: Ensure room doesn’t become too cold in early morning
- Appropriate bedtime: Counterintuitively, an earlier bedtime (7-7:30pm) often helps
- Brief response: Keep early morning interventions brief and boring
- Consistent morning time: Establish a consistent acceptable wake time (typically 6-7am)
- Gradual adjustment: If needed, gradually shift wake time later by 15-minute increments
Supporting Healthy Sleep at 4-5 Months

Build on previous foundations with these age-appropriate approaches:
DO:
- Establish wake windows: Aim for 1.5-2.5 hours of awake time between sleeps
- Use sleep environment consistently: Same crib, sound, darkness for all sleep periods
- Watch total daytime sleep: Ensure sufficient daytime sleep (3-4 hours total) to prevent overtiredness
- Balance stimulation: Provide appropriate physical and mental stimulation during awake periods
- Consider hunger needs: Some babies benefit from cluster feeding before bedtime
- Create clear sleep onset cues: Consistent phrases, songs, or actions that signal sleep time
AVOID:
- Inconsistent timing: Dramatically different schedules day-to-day can disrupt developing patterns
- Skipping naps: Pushing through naps often backfires with overtiredness
- Screen exposure: Especially in the hour before sleep periods
- Overtiredness: Watch for early tired cues rather than waiting for obvious exhaustion
- Overstimulation: Particularly in the final awake window before bedtime
When Sleep Training Progress Stalls
If you’ve been working on sleep training but progress has stalled:
- Reassess approach: Consider if your current method matches your baby’s temperament
- Check for consistency: Ensure all caregivers follow the same approach
- Rule out physical factors: Teething, illness, growth spurts can temporarily disrupt progress
- Evaluate sleep environment: Ensure optimal conditions for sleep
- Consider developmental factors: Motor milestone practice often temporarily disrupts sleep
- Give adequate time: Most approaches need 1-2 weeks of consistent implementation
- Consult your pediatrician: Discuss concerns and rule out medical issues affecting sleep
- Check out this link for more details on the 4-month sleep regression.
Final Thoughts
The 4-5 month old sleep period often marks a turning point in infant sleep development. The biological foundations established during the 4-month progression now begin to manifest as more predictable patterns and sleep capabilities.
While perfect consistency shouldn’t be expected, many families find this period brings welcome relief after the regression and lays important groundwork for healthy sleep habits throughout the first year.
Remember that your consistent response and routine during this period helps your baby build secure sleep associations and strengthen their developing circadian rhythm—valuable skills they’ll carry forward.
In our next post, we’ll cover months 5-6, when many babies consolidate to two longer naps and may be ready for a more predictable by-the-clock schedule.
Disclaimer: This information is intended for educational purposes only and is not a substitute for personalized medical advice. Always consult with your pediatric healthcare provider regarding your specific situation and concerns.







